Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information “There is no such thing as a healthy tan,” says the American Skin Association, which regards any tan as an injury, no matter how beautiful it may look. […]
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
“There is no such thing as a healthy tan,” says the American Skin Association, which regards any tan as an injury, no matter how beautiful it may look. Even after a tan fades, the genetic structure of the affected skin will remain damaged forever more.
Perils of the Sun
“There is no amount of sun that is good for the skin,” says Dr Robert Brodell, professor and chair of the Department of Dermatology at the University of Mississippi Medical Center. So, as we move into spring and summer and longer hours spent outdoors, this is a good time for clinicians across a variety of specialties to reassess the ways they monitor a patient’s largest, most visible organ.
Citing a study from the National Center for Biotechnology Information, Dr Delphine Lee of Harbor-UCLA Medical Center reminded Medscape that something as simple as a mild sunburn can increase the risk for melanoma, the deadliest form of skin cancer.
Luckily, the skin is one organ that clinicians across all specialties are seeing, and this offers a secondary opportunity for prevention and early detection.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share

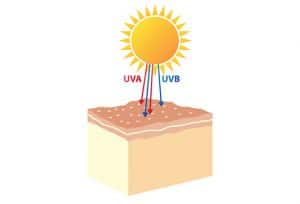
Clinicians can advise patients to pay attention to the UV Index. A reading of 6 or 7 indicates high risk to unprotected skin during sun exposure. Sunglasses that offer 99%-100% protection from UVA and UVB light are best, especially those marked UV 400. [2]
Sunburn
Sunburns, even mild ones, trigger changes in the skin that can result in serious problems in the long term. According to the Skin Cancer Foundation, the rate of skin cancer is now higher than that of all other cancers combined.
Despite so many warnings, many people continue to venture unprotected into the sun and fail to have regular appointments with their dermatologists to boot. In one extreme example of noncompliance, a new and dangerous creative outlet known as sunburn art has cropped up in recent years. It involves wearing stencil-type cut outs to create designs or words on skin via the contrast between burned and unburned skin.
Chances are that if a patient comes in with sunburn, it will not be his or her first. This is a good opportunity to question the patient about previous burns and suggest a visit to a dermatologist for regular screening, says Dr Lee.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share

All sun poisoning will burn, itch, and hurt, but people with fair skin can suffer second- or even third-degree burns in the sun, which can be excruciating and unsightly. Both tanning and burns cause cellular damage and increase the risk for skin cancer, though more extreme burns and sun poisoning pose a greater risk.
Sun Poisoning
Skin can burn in just 15 minutes, and some unprotected skin may even develop sun poisoning in that length of time or soon after. For 4-7 days, people with sun poisoning may have an itchy, burning area of skin that resembles a rash or looks like a cluster of blisters.
Swelling, headache, fever, dizziness, nausea, hyperpnea, rapid pulse, dehydration, and even fainting may also occur. Patients with immediate or recent sun poisoning should be seen by a dermatologist, who may be able to provide treatments that can reduce skin cancer risks.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Sun and ultraviolet exposure greatly accelerate the deterioration of skin appearance and structure over a lifetime.
Photoaging
Skin cancer is the most severe and dangerous consequence of sun damage, says Dr Brodell. However, even those who are lucky enough to escape malignancy still face premature aging and precancerous conditions that can cause issues ranging from the cosmetically undesirable or disfiguring, to the psychologically stressful and expensive.
The “photo” in photoaging derives from the Greek word phos, meaning light, so the word literally means “light aging” or “aging from light.” It is the result of repeated exposures to ultraviolet radiation.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Researchers reported on one 16-year-old patient, a regular user of UV tanning beds, who was referred by her GP due to concerns about potentially malignant changes in her nevi. [3] She is just one of many such cases across the United States, as skin cancer rates are rapidly on the rise in children and teens.
Tanned Skin
There will always be patients who are careful never to burn but still tan throughout the summer or even all year long.
Dr Brodell points out that glowing tans may look great, but that golden hue almost certainly indicates lots of time in the sun, in a tanning bed, or both. This offers an opportunity to have a frank discussion with the patient about risks and easy prevention. Patients can benefit from graphic depictions of the damage and disease that sun exposure can cause. Because tanning appeals to vanity, visual damage may be an excellent warning vehicle for this group.
Some tanners believe that tanning is safer in a tanning bed, so it’s important to dispel this myth and let patients know that indoor tanning may pose an even greater melanoma risk. Even parents need to be reminded of the dangers. According to a recent study published in JAMA Dermatology, daughters are often brought to their first tanning session by their own mothers. [4]
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Atypical mole syndrome puts patients at significant risk for melanoma. Because early detection is critical, these atypical nevi must be closely monitored. [5]
Freckles and Moles
Freckles are triggered by exposure to sunlight, so their presence offers a clue about time in the sun. Skin cancer risk is also higher in those who freckle easily.
Dr Jennifer Stein, of NYU Langone Medical Center and associate director of its Pigmented Lesion Service, says that it is always a good idea to take a more vigorous look at a patient’s existing moles. Although many are benign and will remain that way, a patient who has many moles is at increased risk for melanoma and should see a dermatologist regularly.
The sudden appearance of a brand-new, first mole (especially in a younger patient) also calls for a dermatologic checkup.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Fibroblast growth factor increases cell viability and invokes angiogenesis, which leads to tumor growth. [6]
Actinic Keratosis
Actinic keratosis, or solar keratosis, is a scaly, crusty growth caused by sun exposure. Although precancerous, these lesions could become malignant at any time; they should be excised and biopsied. It stands to reason that a patient with actinic keratoses has spent a lot of time in the sun and should be referred to a dermatologist for regular screening.
According to the Skin Cancer Foundation, actinic keratoses that are left untreated may become life threatening.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
A superficial basal cell carcinoma (multicentric), most commonly found on the trunk (40%) or distal extremities (14%). [7]
Early Basal Cell Carcinoma
A superficial basal cell carcinoma can be confusing to many a clinician. It may look just like a red splotch on the skin at first, flat and unremarkable, or it may be raised. Clinicians who are less familiar with its variety of manifestations may mistake a basal cell carcinoma for eczema or psoriasis. [7]
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
According to Dr Talib Najjar, professor of oral and maxillofacial surgery and pathology, Rutgers School of Dental Medicine, ultraviolet light from sun exposure is a risk factor for cutaneous squamous cell carcinoma, while antioxidants and aspirin may reduce the risk of developing it.
Squamous Cell Carcinoma
A squamous cell carcinoma can look very much like a basal cell carcinoma, but its often scaly nature can differentiate the two. These can be aggressive and lead to metastatic disease.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Merkel cell carcinoma on the right eyebrow. In some cases, it can metastasize to distant organs, including the pancreas. [8]
Merkel Cell Carcinoma
Presenting as cherry-like papules, Merkel cell carcinomas are found primarily on the head and neck, trunk, and extremities, as sunlight exposure is a primary risk for this cancer. It is most often found in older patients.
Merkel cell carcinoma is a rare and aggressive neoplasm with neuroendocrine origins. Local recurrence following excision is common, and distant metastasis is a possibility as well, so it is wise for clinicians to keep a vigilant eye on these tumors. [8]
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
A 20x digital dermoscopy image of melanocytic lesions that appear very similar to one another: (A) compound melanocytic nevus; (B) dysplastic nevus; (C) dysplastic junctional nevus with severe atypia; (D) thin melanoma. [5]
Melanoma

The Skin Cancer Foundation reminds clinicians that the classic ABCDE warning signs of melanoma are: Asymmetry, Border irregularity, Color variations, Diameter over 1/4 inch (6 mm), and Evolution or change.
Melanoma lesions tend to come in odd shapes, with irregular borders. They often contain shades of colors, including blue, black, tan, and red (but can also be colorless). They are usually larger than a pencil head eraser, and, if the mole in question has always existed, changes in shape, size, or color indicate unusual growth.
Atypical moles, or dysplastic nevi, are often indistinguishable from early-stage melanoma and are also at risk of becoming malignant. Patients and clinicians can never be too vigilant when it comes to monitoring moles.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
This solitary nodule, 1.5 x 1 cm, asymmetrical, and originating from a lesion that had been present since birth, was on the right ankle of a 22-year-old woman. She was diagnosed with amelanotic spitzoid melanoma and referred for testing of distant metastasis. [9]
Amelanotic Melanoma
According to the Skin Cancer Foundation, some melanomas have very different features. Most notably, some lesions lack the dark coloring that most often typifies melanoma, and some are entirely colorless. These melanomas are referred to as “amelanotic.” They can be pink, red, purple, clear, or skin color. This presents an extreme challenge because it’s that much harder for patients and clinicians to even see these lesions, much less to recognize that they are dangerous. Even artificial intelligence apps designed to detect early melanoma look for the classic ABCDEs and can miss these subtle threats. To make matters worse, amelanotic melanomas both recur and metastasize more frequently than do melanomas with more typical features.
Patients can still look for changes, asymmetry, and “ugliness” in any skin lesion and do self-examinations every month, head to toe. They should also see a dermatologist for screenings as often as recommended.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Many people do not realize that melanoma can form in the eye, both in areas that can be seen and in those that can only be observed during a more thorough ocular exam. Patients should have regular eye exams for this and other reasons, even if they are not experiencing vision problems or pain. In Expert Review of Ophthalmology, Drs Gündüz and Esmaeli note that early detection of intraocular melanoma is key. [10]
Melanoma Anywhere
Dr Delphine Lee of Harbor-UCLA Medical Center reminds clinicians that sun damage lesions and skin cancers can crop up anywhere, and some areas of the skin’s surface are less obvious. The sclera and iris of the eye are two such locations. Physicians usually look at a patient’s eyes during a routine exam, so this is something to monitor.
The same is true of the scalp, the soles of the feet, and the palms of the hands, says Dr Lee. Those parts of the body are exposed to the sun too. Clinicians may want to recommend to patients that they ask their romantic partners, family members, hairdressers, and massage therapists to mention any new or unusual lesions; they can be in a unique position to identify problems early on.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Pigmented streaks in a nail bed could signal melanoma in a person of any skin color. Although these lesions could be benign, they should be checked by a clinician as early as possible for the best chance of avoiding metastasis of a malignancy. [11]
Cancer Can Strike Skin of Any Shade or Color
Fair-skinned patients are at higher risk for long-term damage, says NYU’s Dr Jennifer Stein, and light eye color is a risk factor as well. It is critical, though, that people with darker skin understand their risks. In some ways, skin cancer is a greater risk to this group because the possibility of getting it is not on their radar. According to dermatologist Maritza I. Perez, MD, a senior vice president of the Skin Cancer Foundation, a study in the Journal of the American Academy of Dermatology [12] showed that melanoma is more deadly in African Americans, who tend to be diagnosed in later stages. Famous reggae artist Bob Marley died of metastatic melanoma when he was 36 years old.
Those with dark skin are more likely to develop melanoma on their palms, soles, and within the nail beds of fingers and toes. The scalp is another area to watch. And although those with darker skin don’t tend to burn, it is still wise to follow the same sunscreen, cover-up, and eyewear rules that those who are fair skinned should be following.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Enjoy the Sunshine Safely, and Find Benefits Elsewhere
Although there may be benefits of the sun beyond the generation of vitamin D, they occur after a very short duration of exposure. Light reduces melatonin levels that can make people feel sleepy and low on energy. It also tends to increase serotonin levels, fighting off the blues. These mechanisms appear to work by stimulating the brain from direct light signals to the retina of the eye. Wearing sunscreen should not prevent the benefits from taking hold.
Vitamin D is important, though. It regulates calcium and phosphorus absorption, maintains healthy bones, and may protect against cancer, multiple sclerosis, and depression. Patients can certainly speak to providers about taking a vitamin D supplement.
Clinicians can help patients overcome objections by listening to their concerns so that sun safety can be a priority.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
Spray tans may appear softer and more even than their sun-damaging counterparts. It is important to remind patients that spray tans don’t offer any sun protection and that adequate SPF should still be used.
Appeal to Vanity to Save a Life
If wrinkles and surgical scars of the future are not enough to sober patients into taking precautions in the sun, clinicians can always appeal to a more immediate vanity issue.
Sunless tanning has come a long way from its orange-palm and tell-tale-streak days. When used several days per week, today’s gradual-tanning formulas darken the skin over several days or weeks so that minor inconsistencies can be easily smoothed out along the way. This suggestion may resonate with some patients.
Spray-tan booths provide a relatively quick full-body tan. These services have become incredibly popular, and the dermatology community is looking closely at how to formulate guidelines for their usage and to gauge safety. [13] Some salons even offer an organic version of the spray tan solution. It is always a good idea for patients to ask about ingredients of any skin product and run them by a dermatologist.
Sun and Skin: From Burns to Melanoma, What Every Clinician Needs to Know and Share
Toni Kamins, MA; Jennifer Leavitt | April 21, 2017 | Contributor Information
In recent decades, sunburn incidence and severity have increased on every continent. [14] Damage to the ozone layer has been one factor, contributing to UV intensity. People need to be more careful in the sun today than ever before.
It May Take a Village
Dr Shawn Allen, Skin Cancer Foundation spokesperson and founder of Dermatology Specialists in Boulder, Colorado, says that providers can educate their patients about the sun’s role as an immunosuppressant and how dangerous exposure can be because of that. It is important to remind people that the sun should be approached with caution and proper protection, he says.
The skin is the body’s most visible organ, and it’s the first thing any clinician sees on a patient. That opportunity could go a long way toward preventing and identifying conditions that can turn deadly. Luckily, we live in an age in which patients have options when it comes to mimicking all of the health and beauty benefits of sunshine. The more often they hear that advice, the more likely it is to foster good habits.

